scar tissue from injections
 Nodules of fibrocollagenous scar tissue induced by subcutaneous insulin injections: a cause of poor diabetic control | Postgraduate Medical Journal
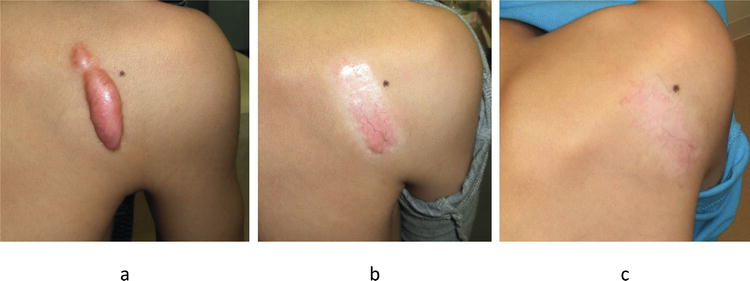
Nodules of fibrocollagenous scar tissue induced by subcutaneous insulin injections: a cause of poor diabetic control | Postgraduate Medical JournalLog in using your username and password Main menu Log in using your username and password You are hereArticle Text Summary A 46-year-old man with type 1 diabetes developed a significant weight loss and a marked deterioration in diabetic control. He had been injecting persistent insulin into areas of abdominal lipohypertrophy within which nodules of hard collagenized fibrous tissue had been developed. Insulin injection in different sites dramatically improved blood glucose control. No fibrocollagenic nodules induced by insulin have previously been described. The examination of 73 other type 1 patients revealed lipohipertrophy in 44% and hard subcutaneous nodules in two. Altmetric.com StatisticsInsulin injections can cause a variety of subcutaneous changes, especially if patients do not rotate sites. This includes lipohipertrophy, lipoatrophy and rarely infections. The widespread use of human insulin has reduced the prevalence of lipoatrophy, but lipohipertrophy remains a significant clinical problem that occurs in 27-48% of patients. Lipohipertrophy can lead to absorption of erratic insulin and is antiesthetical. There are few reports of injection site problems in recent literature. We report a case of a previously undescribed phenomenon of large, hard subcutaneous bilateral nodules in the abdominal wall injection sites. The examination of 73 more patients with type 1 diabetes revealed lipohipertrophy in many cases, two of which had also developed hard subcutaneous nodules. CASE REPORTA 46-year-old male with type 1 24-year-old diabetes presented with an abscess in his scalp. There had been a weight loss of 11 kg and the worsening of diabetic control (hemoglobin glucose (HbA1c) increased from 10.6 to 16.5 per cent) despite a higher dose of insulin over the past 12 months. He had a history of microalbuminuria, peripheral neuropathy, substance retinopathy, cerebrovascular disease and hypertension and took 30 units of human insulin Mixtard 26 twice a day. For years he had given all his insulin injections on the abdominal wall. It had bilateral areas of 8 × 8 cm of typical lipohipertrophy (see fig 1) that both contained 4 cm single diameter nodules of wood that felt like golf balls. He said he always injected insulin into these nodules. The biopsies of the central part of one of the lesions revealed a dense hypocellular and hypovascular collagen with bland-like fibroblasts and necrosis foci. The appearance was that of collagen scar tissue. There was no evidence of amyloid. Abdominal wall injection sites that show bilateral lipohipertrophy areas that contain hard " golf balls" of fibrocollagenic scar tissue. The rotation of injection sites was advised, avoiding nodules and lipohipertrophy areas. In three months the glucaemic control had improved (HbA1c 9.7 per cent), its weight had increased by 10 kg, and the insulin dose had reduced to 38 units per day. Lipohipertrophy areas had been reduced to 2.5 × 2.5 cm and nodules were much smaller and softer. AUDIT OF INJECTION SITES Injection sites of 73 consecutive patients with type 1 diabetes (48% male), mean age 31, mean duration of diabetes 13.6 and mean HbA1c 9.5% were examined. Thirty-three patients (45%) had not examined their injection sites during their last annual examination. Most patients (42) reported rotating insulin injection sites on a regular basis, while 31 patients tended to stick to a main area, although the rotation within that area was reported. The most common sites for insulin injections were legs and abdomen. A total of 32 patients (44%) had clinical lipohipertrophy (armas 41%, legs 31%, more than a site 28%). Twenty-five were described as diffuse, five as a minor induration, and two patients had hard nodules inside hypertrophid areas (an abdominal and a thigh). One of these patients had very poor diabetic control (HbA1c 14.6%) and a recent weight loss and also admitted to repeatedly injecting into the hard nodules. There was no significant difference in HbA1c between those with lipohipertrophy and those without (9.6% v 9.5%). The mean duration of diabetes was significantly higher in those with lipohipertrophy than those without (17.2 (9.2) v 11 (7.1) years, pThe three patients with hard nodules (including index case) were injecting human insulin. DISCUSSION Previous studies of insulin injection sites have not reported large discrete nodules of fibrocholagenic cicatricial tissue, although there is a report of a hard thigh node containing amyloid. Our audit identified two other patients with similar hard nodules, both had poor diabetic control (HbA1c 14.4% and 11.1%), and one had weight loss similar to the index case. It is reasonable to assume that the repeated trauma of localized subcutaneous injections can lead to fat necrosis and then nodules of fibrocollagenic scar tissue. These nodules would not be very vascular and the injection in them would lead to insulin release with deficiencies and poor diabetic control. In our patient index there was a notable improvement in glucaemic control and weight gain after the rotation of insulin injection sites and shrank hard collagen nodules. The three patients with hard nodules admitted to injecting all insulin injections into nodules mainly due to custom and comfort despite having previously been informed of the importance of the rotation of insulin sites. Curiously, abdominal nodules were only perceptible to the two patients after a rapid weight loss and were more evident when standing. Lipohipertrophy of the injection site remains a significant problem in our clinical population with 44% of patients surveyed with some degree of lipohipertrophy. Prevalence rates reported above range from 27% to 48%, with higher rates reported in type 1 diabetes than type 2 insulin diabetes. As with several previous studies we find no significant difference in glucaemic control between those who have lipohipertrophy and those who do not have lipohipertrophy. Lipohipertrophy was associated with a longer duration of diabetes and some of these patients may have been initially treated with animal insulin. It is disappointing that almost half of our patients (45%) would not have had their injection sites examined in the last annual review, although this is recommended. Learning points Lipohipertrophy is a common complication of insulin subcutaneous therapy. Hard fibrocollagenic nodules can occasionally be found in lipohipertrophy areas and may be associated with poor diabetic control. Patients should be advised to rotate injection sites preferably avoiding the same skin patch for a month. Injection sites should be examined at least annually and more often if diabetic control deteriorates. Many of our patients with lipohipertrophy were aware of the importance of rotating insulin injection sites, but cited the habit as the main reason they continued to inject in the same area. It has been shown that the avoidance of sites with lipohipertrophy improves glucaemic control, so it is necessary to incorporate repeated advice on the organized rotation of insulin sites in patient education programs. Persistent injections in lipohipertrophy areas can lead to fibrocollagen scar tissues " golf balls" and cause significant deterioration in diabetic control. REFERENCE Request for permissions If you wish to reuse any or all of this article, please use the link below that will take you to the RightsLink Service of the Copyright Settlement Center. You will be able to get a quick price and instant permission to reuse the content in many different ways. Copyright Information: Read the full text or download the PDF: Sign in with your username and passwordOnline: ISSN 1469-0756Print: ISSN 0032-5473 Copyright © 2021 Postgraduate Medicine Fellowship. All rights reserved. 4.00ICP sponsors15042040 forwarded-3

Lipohypertrophy causes unexplained highs and lows - Diabetes Voice

8 Injections That Heal Injuries | T Nation

The Dangers and Difficulties of Insulin Lipohypertrophy
Update on hypertrophic scar treatment

Botox Injections Found to Be an Effective Facial Scar Treatment | Allure

Scar tissue: Causes, prevention, and treatment

How to Prevent Scar Tissue from Insulin Injections

scars

Scar Tissue Development After Gynecomastia Surgery - Dr. Caridi Explains

Management of Keloids and Hypertrophic Scars - American Family Physician

Steroid Injections for Raised Scars : What You Need to Know | Biodermis.com

WARNING: SCAR TISSUE from TESTOSTERONE INJECTIONS - YouTube

Best Treatment Option for Keloid Scars or Scarring

The Dangers and Difficulties of Insulin Lipohypertrophy

Lumps And Bumps From Insulin Therapy | The LOOP Blog

Picture of Hypertrophic Scar on MedicineNet

Scar - Wikipedia

Facial and Body Scarring - New York, NY | Lipostructure Fat Grafting

Breakdown Of Scar Tissue - Benefits Of Massage - Massage - Treatments - Physio.co.uk

Breaking Down Scar Tissue Using Proven Chiropractic Techniques – Chiropractic BioPhysics

Scar tissue pain: What it feels like, why it happens, and treatment
AMICUS Illustration of amicus,injury,muscle,strain,injuries,treatment,stretched,torn,swelling,impingement,adhesion, scar,tissue,SI,joint,injection,pain,back

Keloids - Harvard Health

How To Get Rid Of Keloids - Treatment | familydoctor.org
Keloids and Hypertrophic Scars Can Now Be Treated Completely by Multimodal Therapy, Including Surgery, Followed by Radiation and Corticosteroid Tape/Plaster | IntechOpen

Botox Injections Found to Be an Effective Facial Scar Treatment | Allure

Adhesiolysis

Cortisone: The end of an era
OT] is this scar tissue? - Bodybuilding.com Forums

Body Piercing Scars | Painfulpleasures Inc
/GettyImages-161140672-56cf8efb5f9b5879cc663e84-5dc51c0134d047258be559df678b53cb.jpg)
Insulin Injection Sites: All You Need to Know

Insulin injection site dystrophic calcification with fat necrosis: A case report of an uncommon adverse effect Ramdas S, Ramdas A, Ambroise M - J Fam Med Primary Care

Scar Tissue from Ankle Injuries | Mercy Health Blog

Hypertrophic Scar: Treatment, Causes, Image, and More

Dermal fillers for scars | Melior Clinics
Bigbobs "Delt lumps are scar tissue not synthol"

Treatment of keloid scars with intralesional triamcinolone and 5-fluorouracil injections – a randomized controlled trial - Journal of Plastic, Reconstructive & Aesthetic Surgery

Pioneering stem cells treatment saw damage reduced by 40% compared with 10% | Daily Mail Online

Keloid and hypertrophic scar | DermNet NZ

Current Concepts In Treating Hypertrophic Scars And Keloids | Podiatry Today
Posting Komentar untuk "scar tissue from injections"